Project and Studies
Protecting Reproductive Information Sharing Mechanisms (PRISM)
We’re hoping to better understand how people interested in childbearing find reproductive healthcare information, what resources are most helpful, where there might be gaps, and any concerns around privacy and access to information.
Thank you for your interest in the Protecting Reproductive Information Sharing Mechanisms (PRISM) research study! Your insights will help shape a curriculum or program to better support reproductive healthcare in our community. The screening survey here will help us decide if you are eligible to participate in our study. Completing this survey does not constitute participation in the study itself. Responses to this screening survey will be stored until this study is complete. After the study is complete, we will delete these screening responses.
Using interprofessional education to transform health services so that each birthing person, and health team member is seen, heard, and valued
More people in the United States die in childbirth than in other wealthy countries. Black women in the United States are dying at a higher rate compared to more than 100 countries worldwide. Structural and social determinants of health are the root causes of health inequities in systems. Many health models focus on fixing individual problems instead of these larger, root causes.
We are working with communities, clinicians, and other healthcare workers to understand and address structural and social determinants of health. This type of system change requires a multidisciplinary model of care. BELIEVE is focused on developing interprofessional training that prevents and helping to heal medical and workplace traumas experienced by birthing people, families, and healthcare workers.
The overall goal of our work is to transform health services so that each mother, birthing person, and health team member is seen, heard, and valued.
AHA-HERN Annual Meeting ’24 Poster:
Patient and provider experiences of maternal healthcare (PDF)
Jasmine L. Garland McKinney, Kristin Tully, Amelia N. Gibson, and Kimberly D. Harper
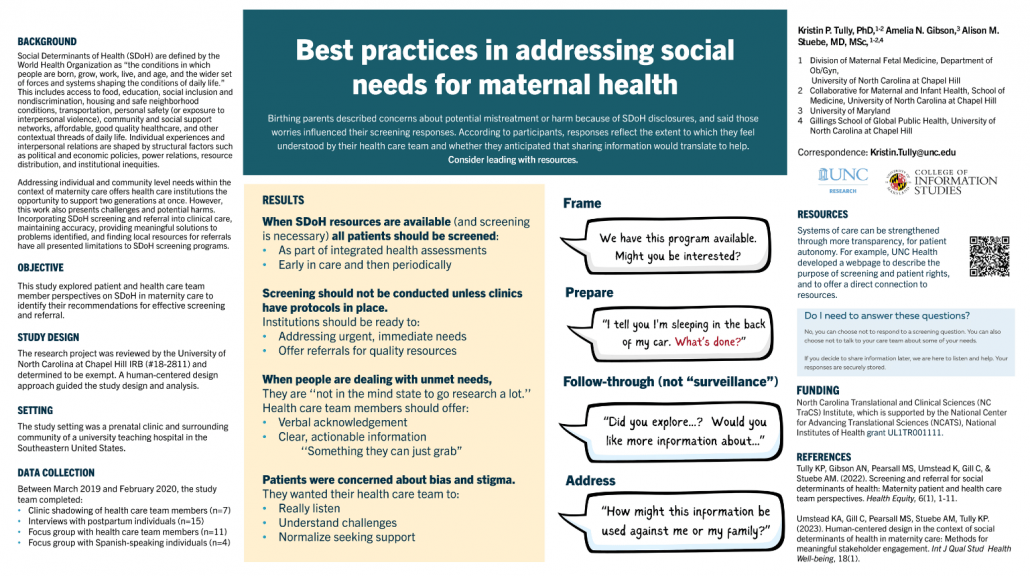
AHA-HERN Annual Meeting ’23 Poster:
Best practices in addressing social needs for maternal health (PDF)
Kristin Tully, Amelia N. Gibson, Alison Stuebe
Black Maternal Health Conference, Black Mamas Matter Alliance ’24 Poster:
Building Equitable Linkages with Interprofessional Education Valuing Everyone (BELIEVE): Amplifying Reproductive Justice through a Novel, Interprofessional Medical Curriculum (PDF)
Jasmine L. Garland McKinney, Kristin Tully, Amelia N. Gibson, and Kimberly D. Harper
Shades of Blue: Breaking Maternal Mental Health Barriers ’24 Poster:
Valuing the mental health needs of Black birthing persons
Jasmine L. Garland McKinney, Kristin Tully, Amelia N. Gibson, Kimberly Harper, Alison Stuebe
Postnatal Patient Safety Learning Lab
Redesigning systems of postnatal care to better enable all families to thrive
To be safe and well, birthing mothers need to be listened to, respected, and experience timely, risk-appropriate postnatal healthcare. However, care can be inequitable and undermine the people and outcomes it seeks to support. This project is about identifying strengths and opportunities to re-engineer postnatal care, to transform process and outcomes for families and those serving them.
This project is a transdisciplinary collaboration across UNC Chapel Hill, NC State University, and Ohio State University to transform postnatal care. Our aim is for our work to be inclusive, effective and inspirational. Our vision is to outline, test and redesign systems of postnatal care in partnership with patients and health care team members to better enable all families to thrive.
This project was funded under grant number R18HS027260 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS). The authors are solely responsible for this abstract’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this reporting as an official position of AHRQ or of HHS.
AHRQ PSLL 2023 Annual Meeting Poster:
What does “safe” mean to patients? Birthing parent definitions of safety in childbirth and postpartum care (PDF)
Amelia N. Gibson, Kristin Tully, Alison Stuebe
This study examined prenatal, perinatal and postnatal care in North Carolina. The purpose of this research study (which was funded by a subaward from the North Carolina Department of Health and Human Services) was to collect stories from 250 pregnant and birthing parents in North Carolina, analyze them for emergent themes related to access, information, and care experiences, and share them with families, the research community, and clinicians to raise awareness and improve support for birthing parents.
We envision a world where every woman receives the social, emotional, physical, and economic support she needs to successfully transition through the postpartum period and into her new identity and life as a mother. Health care systems, businesses, and society should value and respect women not only for what they bring to families, communities, and nations but also for who they are in and of themselves.
Publications
Tully, K. P., Gibson, A. N., Pearsall, M. S., Umstead, K., Gill, C., & Stuebe, A. M. (2022). Screening and Referral for Social Determinants of Health: Maternity Patient and Health Care Team Perspectives. Health Equity, 6(1), 887–897. https://doi.org/10.1089/heq.2022.0020
Deaton, J. D., Borders, L., Wachter Morris, C., McKinney, J. L., Fantahun, S., & Smith, A. N. (2023). Rural Teachers’ Burnout, Well-Being, and COVID-19 Related Stress During the Pandemic. The Rural Educator, 44(4), 29-42. https://doi.org/10.55533/2643-9662.1336
Policy Briefs
Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm
Transparency, and Information Sharing
Public Comment: Black Health Informatics Working Group at the Black Health Heritage Data Lab, Brown University , HHS-ONC-2023-0007, HHS-ONC-2023-0007-0001, 2023-07229 [PDF]
Recommendations for HIT standards. Excerpt:
“Overall, we believe the proposal to enable a certified health IT user to implement a process to restrict data from use or disclosure in response to
a patient request in an effort to support the HIPAA Privacy Rule’s “right to request a restriction” on uses and disclosures is a step in the right direction. It provides patients with an Internet-based option to request restrictions on sharing their USCDI data with external covered entities beyond their clinical or provider’s office. However, we are concerned that patients may not be adequately informed about their right to flag and request restrictions for specific data elements in their medical records (and the fact that these requests may be denied). In addition, it is not clear in the proposed rule that the covered entity needs to explain the patient restriction, specifically whether patients can to request to restrict their data in multiple ways and with different levels of granularity (rather than just having the binary choice to either share or to not share data globally), and if and how patients should be informed about these options.”
NEWS & PUBLIC HIGHLIGHTS
Health Care Barriers: Screening and Referral for Social Determinants of Health in Maternity Care
A Q&A with INFO Associate Professor Dr. Amelia Gibson was recently published in the iSchool News in July 2023. Read to learn more about a recent study about screening and referral for SDoH in maternity care and health equity in maternal health care.
Dr. Jasmine L. Garland McKinney is featured on Assessment Talks, the Association for Assessment and Research in Counseling podcast
Dr. Garland McKinney talks about her work developing the Prepartum Form for Evaluating Race Related Psychological Stressors (PP-FERRPS)©, which assesses stress and anxiety in Black pregnant women. Listen to the episode here.