The American Heart Association has granted $20 million to create the Health Equity Research Network (HERN) through the P3 EQUATE Network at the University of Alabama. This network focuses on understanding contributors to maternal mortality and morbidity among women of color (with a special focus on Black and Native American birthing people). About half of these problems are related to the heart and blood vessels, so the American Heart Association is in a good position to help solve this important issue.
BELIEVE is a $2.4 million HERN grant to UNC Chapel Hill, which includes a $438,000 subaward to the University of Maryland.
The BELIEVE team is led by Kimberly Harper and Alison Stuebe at the University of North Carolina at Chapel Hill, and Janiya Williams at North Carolina Agricultural and Technical University. The core research team includes faculty, staff, and student researchers from UNC Chapel Hill (Chapel Hill, NC), UNC Healthcare (North Carolina, statewide), NC A&T (Greensboro, NC), the University of Maryland College of Information Studies (College Park, MD), Cone Health (Greensboro, NC), and Reaching Our Sisters Everywhere (Atlanta, GA). At UMD, this work is led by Amelia Gibson, Associate Professor at the College of Information Studies and director of the Community Equity, Data & Information (CEDI) Lab.
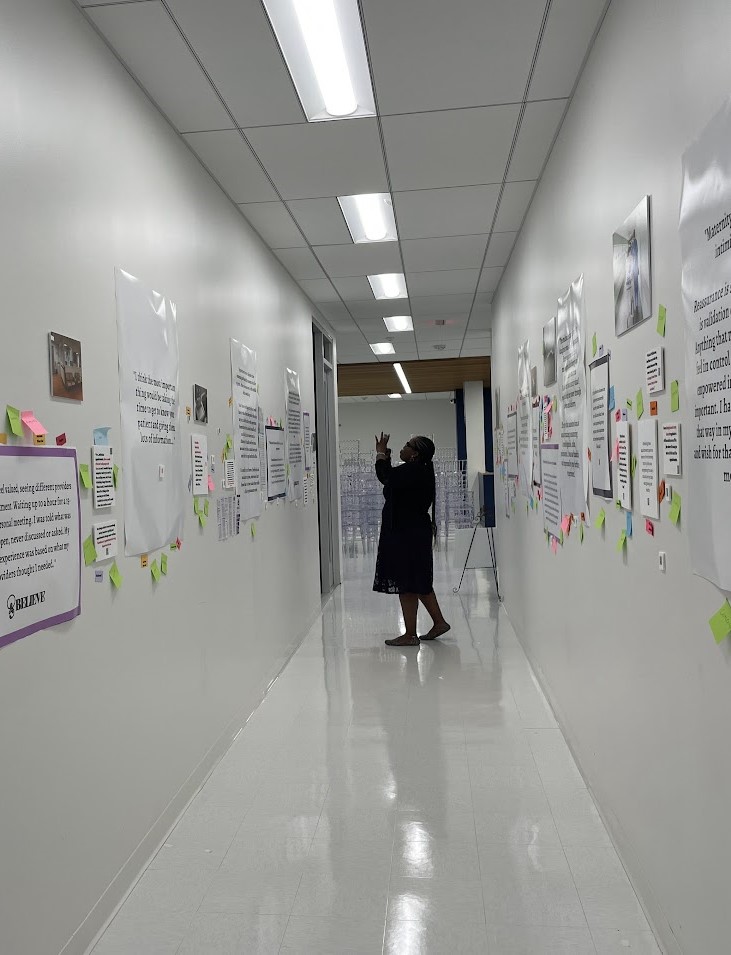
The overarching goal of our work is to transform perinatal and reproductive health services so that each mother, birthing person, and health team member is seen, heard, and valued. The purpose of this project is to develop a curriculum for interprofessional education and collaboration that cultivates trust among birthing people and health team members through respectful, equitable and person-centered care and communication. Using Kern’s six-step approach to curriculum development, we will develop, implement, and evaluate BELIEVE, an interprofessional education (IPE) curriculum for mothers, birthing people, and members of the health care team. Using a stepped-wedge design, we will quantify BELIEVE’s impact on health team members, provider-patient interactions, and health care processes and outcomes.
In 2020, a Black birthing woman in the United States was 2.9 times as likely to die as a non-Hispanic white woman. The maternal mortality rate for Black women in the United States was 55.3 deaths per 100,000 live births, exceeding national maternal mortality rates in more than 100 countries worldwide; for Black infants, the mortality rate of 10.6 per 1000 live births exceeds more than 80 countries. Remediating these disparities, which are rooted in structural racism, require holistic solutions that address “cultural norms, policies, institutions, and practices that define the distribution (or maldistribution) of social determinants of health,” through collaborative, multidisciplinary, multilevel models of maternity and perinatal care. Moreover, building more just, equitable care requires healing the trauma experienced by families, birthing people, and health care team members, diminishing trust, damaging relationships, and leading to poor health outcomes.
Go to the BELIEVE website.
View the BELIEVE Instagram.